What are wider determinants of health and why do they matter so much? Andi Orlowski spoke on the subject at the Together for Health conference for local authority leaders in April 2021, where he explained their importance to all parts of the public sector and the barriers that need to be overcome before truly integrated working can be achieved.
In the past few years there has been a rapidly increasing awareness of the fact that an individual’s health is about so much more than their interaction with GPs or hospitals.
Systematic variation
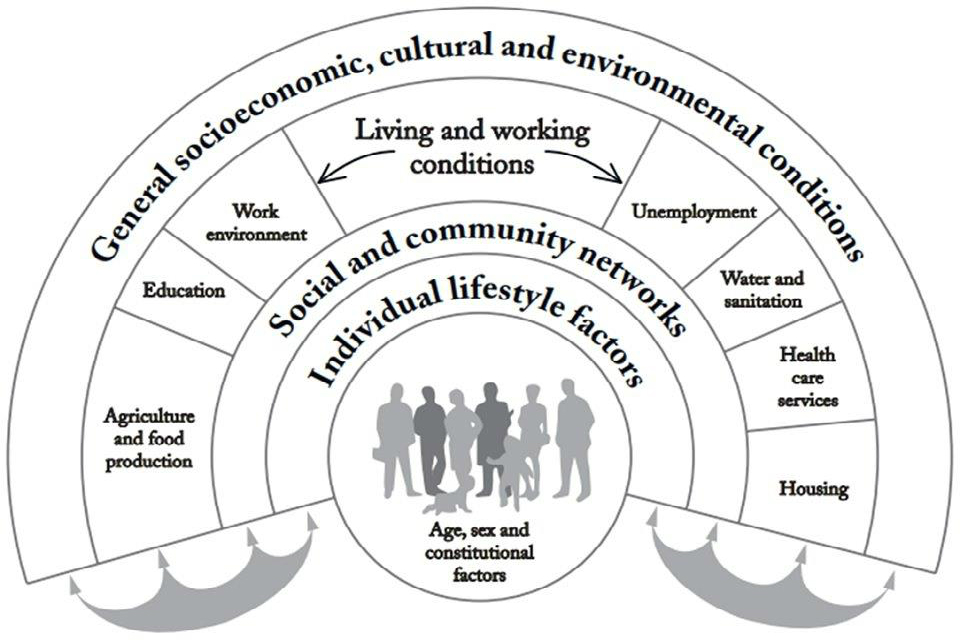
Studies have proven that 80% of a person’s health outcome is determined by non-health related inputs – for example, things like their housing, their finances, their education, their job or their access to green spaces can all play a huge role in how healthy they are. It’s why some of the country’s most deprived communities have been among the hardest hit by the COVID-19 pandemic.
And it is why these “wider determinants of health” are now a key focus of Government policy, with the new Integration and Innovation white paper placing an increased emphasis on prevention and tackling the underlying cause of health inequalities.
Population health management is the big hot topic in the NHS; everyone’s talking about it, but it’s at the very core of the work the Health Economics Unit (HEU) have been doing for many years – using population data and analytics to give local authorities and the NHS a broad picture of all the different factors that may be affecting their populations.
Decisions that the Government and wider public services take every day, about every aspect of a citizen’s life, have a direct impact on public health, and people are more aware of this now than they have ever been.
In my talk at the Together for Health conference I welcomed this increased awareness, but explained that changes can only be made if all parts of the public sector pull together – this is not simply a problem for the NHS to tackle in isolation.
Partnerships for success
The NHS cannot do this by itself; it has to work alongside local authorities and government departments to be able to solve the problem – only then will true differences start to be made.
Access to care is an important part of overall population health. We also need concerted action in areas such as income security, education, housing, nutrition and the environment.
There are only very marginal gains to be made by tackling the health part of the equation and it would be wholly inappropriate to start dragging it back to the 20%, when we will achieve far more by focusing on the 80%. But this is where the challenge comes – the NHS cannot work in isolation here and these wider determinants should not be over-medicalised.
In order for real systemic change, all partners need to be sharing the responsibility. It’s about looking at how we work with the money we’ve got and how this can be shared across the entire system in order to gain maximum benefits.
Resources that currently sit within the NHS need to be moved out into these wider areas – but this is going to involve a complete culture change and needs some key changes to happen in order for it to work. As things stand at the moment, which NHS trust is going to be brave enough to give away big chunks of money?
Moving money from one pot to another will often result in savings, and a better overall experience for the public, but the savings might happen in the system, rather than in the hospital, and the hospital trust then loses out.
A truly integrated approach
For truly integrated care that effectively addresses the wider determinants of health a huge amount of work needs to be done to address these issues. There has to be a way of looking at the finances at a system level to ensure that when you move the money out of your organisation it’s somehow managed to make sure you don’t lose out. What will these mechanisms be? If you give your money away, how do you get it back?
The changes needed in order for true collaboration will not be easy. There is a lot of hard work that has to happen, but I am convinced it can and it will. There are some fantastic examples already taking place in some areas – a few of which I outlined in my talk at the conference:
- A ‘boilers on prescription‘ scheme run by North East-based housing firm Gentoo Group and Sunderland Clinical Commissioning Group where boilers, double-glazing and insulation were supplied ‘on prescription’. A&E attendances reduced by 30%. Emergency admissions reduced by 25% and GP appointments reduced by 60%.
- Guy’s and St Thomas’s Hospital Trust in London paying £250k to fund Low Traffic Neighbourhoods to tackle air pollution and obesity in Lambeth and Southwark.
The HEU team is keen to work in collaboration with organisations across the NHS. To find out more about how you can get involved, please contact us.
Author: Andi Orlowski
 Andi Orlowski is a health economist and the Director of the Health Economics Unit. Andi is passionate about population health analytics, especially about addressing health inequalities. He is researching this for his PhD at Imperial College London.
Andi Orlowski is a health economist and the Director of the Health Economics Unit. Andi is passionate about population health analytics, especially about addressing health inequalities. He is researching this for his PhD at Imperial College London.